If your goal is to manage PCOS, you need to understand that the factors and symptoms you have are unique. PCOS is different for everyone. What triggers your PCOS symptom is not just sugar or missing a gym session or the exam week. This blog post contains information available online from various sources and does not constitute a medical opinion or advice. While medications should only be taken based on a doctor’s advice, one can start with a natural approach to managing PCOS.
PCOS is a syndrome. Unlike a disease that has a specific cause, symptoms, and treatment, PCOS does not have a well-defined cause and treatment. Instead, Doctors identify PCOS when concurrent symptoms are often seen together. The exact cause of PCOS remains a mystery. Therefore, a cure for PCOS is not yet available. Presently, the treatment of PCOS is about reducing its symptoms.
Factors that Causes of PCOS
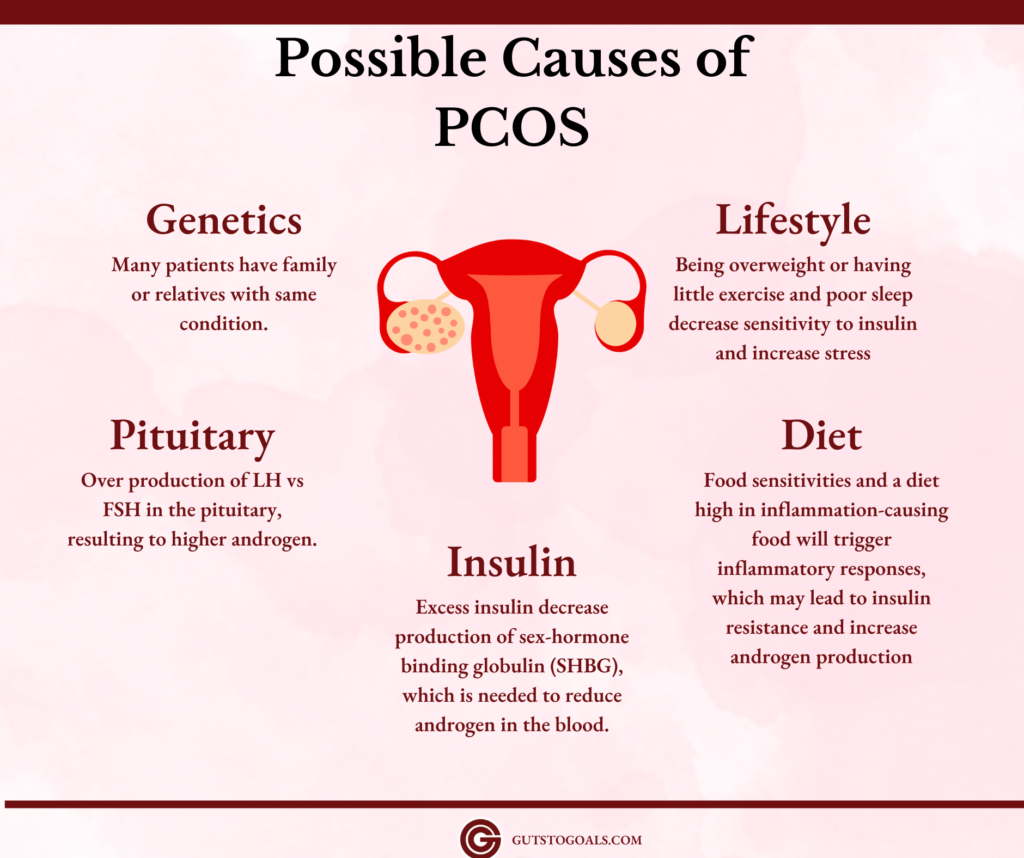
Medical researchers are looking at a combination of genetics, food intake, and environmental factors. The only thing certain is that PCOS patients suffer from hormonal imbalance -especially high luteinizing hormones (LH) and insulin, which causes an increase in androgen levels. Therefore, combating PCOS means the management of these hormones.
Normally, LH stimulates the ovaries to produce eggs. However, too much LH results in overstimulation and excess estrogen. The ovaries will then convert it to androgens, which causes more follicles to grow into cysts but never mature into an egg (causing polycystic ovaries). Higher LH may result from insulin resistance, pituitary disorder, eating disorders, inflammation, and even stress. Note that PCOS cysts have immature eggs inside, unlike the usual cyst.
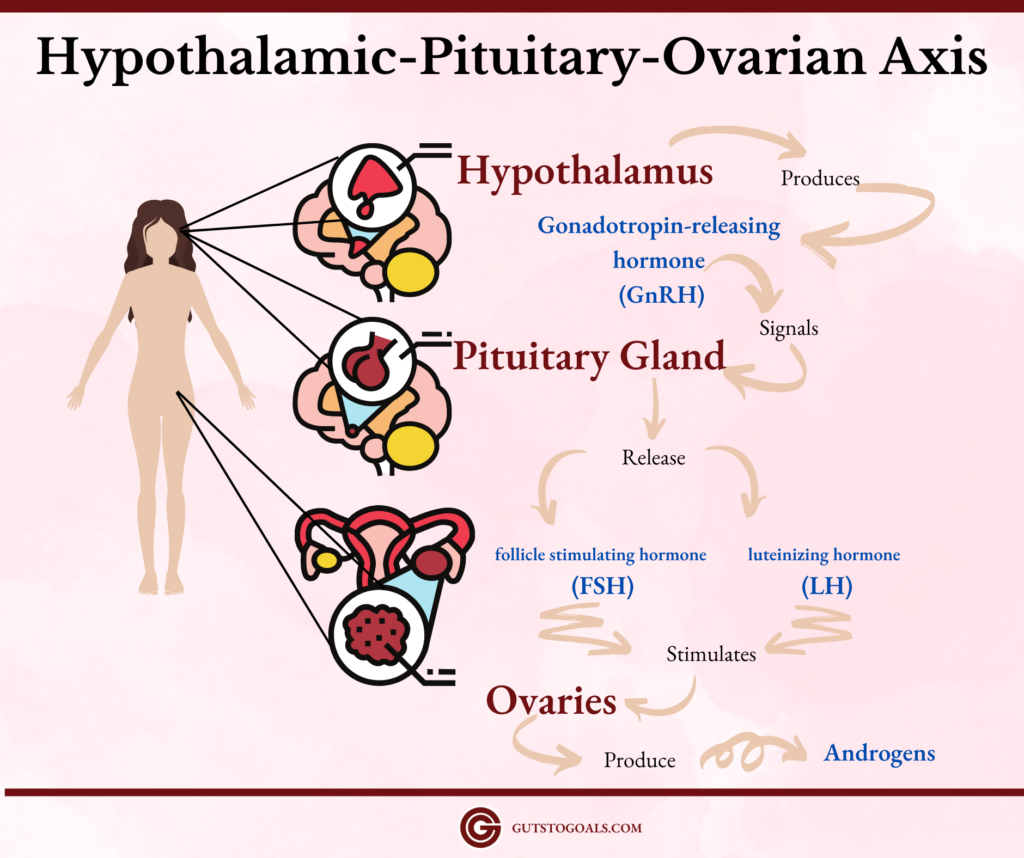
The Hypothalmic Pituitary Ovarian Axis regulates women’s reproductive system. Below is a quick illustration of how it works.
Common Ways to Manage PCOS
High androgen levels can be controlled by Spironolactone and Hormonal birth control pills. Spearmint tea can help reduce testosterone, so as licorice, peony, almonds, and green tea.
Infertility issues are managed by giving clomiphene and letrozole to trigger ovulation. If oral treatments fail, your doctor may suggest gonadotropins shots and ovarian drilling. When all else fails, In vitro fertilization or IVF is recommended if the patient wants to be pregnant.
Manage PCOS based on Type or Trigger
Not all PCOS remedies online may apply to your PCOS. Some may be unnecessary and others can even make your condition worse. It is better if you will seek the advice of your doctor to narrow down the possible cause and type of PCOS that you have.
Note that while it is possible to treat (improve) symptoms of PCOS, they may come back any time or when triggered. Hence, PCOS management is a lifetime commitment. Below are the suggested management based on PCOS type and causes.
Manage Insulin-type PCOS
High insulin can cause PCOS, but it is also a symptom. If your family has a history of diabetes, consider getting a blood test for fasting glucose and fasting insulin. The normal levels would be 10 for insulin and 90 or lower for blood glucose.
A factor in Insulin Resistant PCOS is ectopic fat deposition or the accumulation of fat in non-adipose tissues. It happens when there is a dysfunction in adipose tissues related to obesity, lack of physical activity, and genetics. But in women with PCOS, it may result from hyperandrogenemia and hyperinsulinemia. According to a 2011 PubMed article, women with PCOS have hypertrophic adipocytes and impaired lipolysis. Such impairment is seen both in obese and non-obese women and is an early symptom of insulin resistance.
Medical
If you have insulin-resistant, the best course of action is to improve your body’s insulin sensitivity. Doctors may prescribe metformin. However, it is not recommended for those with a sensitive stomach, with kidney or liver failure, or at risk of developing lactic acidosis. Additionally, you should not try fasting or a low-carb diet or taking other insulin-lowering supplements or drugs when you are taking metformin. Otherwise, you might experience hypoglycemia or blood sugar falling too low. Another side-effect of metformin is Vitamin B12 deficiency, so your doctor may recommend taking up B12 supplements.
Since insulin resistance can lead to obesity, the doctor may also prescribe Orlistat (Alli, Xenical).
Diet and Supplements
To increase your insulin sensitivity more naturally, you may ask your doctor about natural insulin-sensitizing food or supplements. The most popular natural supplement is cinnamon. You can easily add cinnamon to your diet.
Studies have found that 3 grams (about 1 tsp) of cinnamon powder can lower blood glucose and cholesterol. Just be careful in consuming it in high amounts. Opt for Ceylon Cinnamon because it is less toxic.
Other insulin-sensitizing foods are pumpkin seeds (high in magnesium and fiber), okra (Rhamnogalacturonan), and fiber sources (like oatmeal, chia seeds, and psyllium husk). Among the herbs and spices, a 2019 study shows turmeric has positive effects on fasting blood glucose.
According to different studies, some supplements can help improve insulin sensitivity. These are magnesium, probiotics (L. acidophilus), and omega-3. In the case of Inositol, those with insulin resistance will benefit from the 40:1 ratio of Myoinositol and D-chiro inositol -often with folate. On the other hand, berberine works by limiting fat storage and improving leptin levels (a hormone that decreases hunger).
Lifestyle
Regular exercise can also improve insulin sensitivity because our muscles require insulin to process glucose (sugar). You should pay close attention to your belly fat (visceral fat) because it can increase insulin resistance. Adding short high-intensity interval training or HIIT three times a week is recommended.
When adding exercise to your daily regime, remember to also increase your fluid intake (3 liters) because it is responsible for maintaining cell stability and transporting nutrients. Note that high insulin levels in our blood can already cause dehydration. So, if you exercise you need to replenish the fluid you are losing asap.
If you are not taking metformin or a strict low-carb diet, you may consider fasting for 12 hours. As much as possible, do not eat three hours before bedtime. On top of these, aim for 6-8 hours of sleep every night.
Other Considerations
As women mature, the level of female hormones (estrogen and progesterone) drops. However, if there is insulin resistance, there is a possibility of developing estrogen deficiency or consistently low estrogen. This will likely cause lighter and shorter periods. Among the symptoms of estrogen deficiency are headache before the period, trouble sleeping and concentrating, and vaginal dryness.
Manage Synthetic (Post-pill) PCOS
In a 1976 article, MS Nakamura explained that Post-Pill syndrome refers to ovulatory disorders experienced by women after taking the birth control pill. The most common effects are a sudden surge of acne, amenorrhea (absent period), headaches, and infertility. This is often reversible and may eventually resolve on its own among women with no PCOS.
Another synthetic source of estrogen that artificially raises its level in women’s bodies is endocrine-disrupting chemicals or EDCs such as Bisphenol A (BPA) and some types of phthalates. Most PCOS women have a higher amount of BPAs in their system than their non-PCOS counterparts. Xenoestrogens (another term for EDCs) affect the genes related to fat accumulation and disrupt the balance between androgen and estrogen in women.
Medical Treatment
Women with PCOS are often prescribed contraceptives to regulate their estrogen and progestin to normal levels. By adding estrogen and progesterone, the androgen levels would remain low. Estrogen contraceptives can stimulate the liver to reduce the amount of testosterone in the blood. Subsequently, it can help control hirsutism and hormonal acne among women with PCOS.
However, when you stop taking the pills, your hormones will be off-balance, mostly increasing androgens (especially testosterone) and insulin. Among women with PCOS, the excess testosterone and/or insulin might be converted into estrogen. Consequently, it will elevate estrogen levels. When there is estrogen dominance, the menstrual cycle can become longer and heavier, fibroids may develop, breast tenderness, and fat may accumulate in the hips and mid-section.
Dr. Stacy Sims mentioned in her blog that oral contraceptives also result in very high levels of oxidative stress. Long-term use of hormonal pills may lead to cardiovascular illnesses or even cancer. Note that those with migraine with aura should avoid taking birth-control pills with estrogen because of the possibility of blood clots, as per the American Migraine Foundation.
Diet and Supplement
You may reduce estrogen in your system by limiting dairy and alcohol for at least 6 weeks. You may also incorporate a liver-detoxifying diet. Simply adding berries, broccoli, and citrus fruit can gradually reduce oxidative stress. Isabel Smith, a certified Dietician, and Nutritionist suggests eating food that promotes progesterone. Magnesium-rich food such as black beans and L-arginine-rich food such as turkey and pumpkin seeds are highly recommended. Adding food rich in phytoestrogens such as flaxseeds and soy can help in transitioning off the pill.
Kresser Institute noted that oral contraceptives can deplete the levels of zinc, magnesium, and vitamin B6. Therefore, supplementing with these nutrients can help improve PCOS triggered when coming off pills.
Among the teas, dandelion root tea can help detoxify the liver. Licorice and Paeonia are herbs that can lower serum and free testosterone among women with PCOS. Supplements like milk thistle can help the body remove excess hormones.
Always consult with your doctor when trying new supplements to manage PCOS. Do not try everything (all supplements) at once. There can be negative interactions among them, which may make them ineffective or even worsen your health.
Lifestyle
As mentioned above, xenoestrogens are synthetic chemicals that mimic estrogen. Most birth control pills have xenoestrogen. Unfortunately, xenoestrogens are stored in our fat cells (long-term storage). Therefore, it can stay in our system for a very long time and disrupts the hormonal balance.
If you recently decided to stop taking birth control pills or if you are experiencing symptoms of synthetic PCOS (such as estrogen dominance), it might be caused by xenoestrogens in your environment.
Plastics, cosmetics, shampoo, lotions, perfume, air freshener, pesticides, and even meat from farmed animals are possible sources of xenoestrogen. Thus, anyone with PCOS or someone who simply wishes to discontinue oral contraceptives should avoid or limit xenoestrogens.
In some cases, hormonal pills can also lead to weight gain or even obesity. Moderate aerobic exercise 2-3x per week may help improve your post-pill metabolism. However, start with gentle exercises like yoga and walking before doing more intensive exercises.
While it is tempting to go on a diet, undereating or restrictive diet can mess up your hormones even more. So keep a balanced diet instead. While a balanced diet may differ from culture to culture and the availability of food in your area, consider cutting down on high glycemic index foods in general.
Finally, if your hormones are disrupted, so is your circadian rhythm. To get it back to normal, limit your screen time and have consistent sleeping hours. As soon as you wake up, expose yourself to natural light and get going.
Manage Inflammatory PCOS
Chronic inflammation drives the ovaries to increase the production of testosterone. To manage PCOS caused by inflammation, the best way is to find the cause of inflammation. In most cases, this is related to food sensitivity (such as gluten and dairy). In others, obesity or lifestyle factors (smoking) can trigger inflammation.
Another common inflammation often ignored is periodontal inflammation. There are studies that show higher periodontal diseases among PCOS women than controls.
If you have a chronic inflammatory disease, it would help if you seek treatment for that condition first. Some examples of chronic inflammatory diseases are fatty liver disease, endometriosis, asthma, and arthritis.
Medical Treatment
Most women with inflammatory PCOS are given probiotics as the first line of treatment. This is because our digestion affects the absorption of nutrients in the body. If our gut’s microbiome is in dysbiosis (low diversity), then we can expect problems such as inflammation, leaky gut syndrome, probably an increased risk of diabetes, and even the development of cancer.
In a 2020 study, Gonzales and colleagues discussed the promising effects of salsalate -a nonsteroidal anti-inflammatory drug NSAIDs (related to aspirin) on those with inflammatory PCOS. They concluded that it can “suppress inflammation, ameliorates ovarian androgen hypersecretion, and may induce ovulation while maintaining insulin action”. Future studies can shed light if salsalate can manage other types of PCOS.
Diet
Apart from probiotics supplements, we can incorporate food with probiotics such as kimchi, yogurt, kefir, kombucha, miso, etc. Adding prebiotics or fiber-rich food can help good bacteria thrive in our guts.
An anti-inflammatory diet excludes sugary and processed food. To combat inflammation, you can add oily fish, dark-colored fruits, green leafy vegetables, beans, nuts, and seeds to your diet. Instead of using white rice, potatoes, and flour, opt for more complex carbohydrates like sweet potatoes and brown rice.
Additionally, you can incorporate turmeric and ginger into your food. Other anti-inflammatory foods are almond, chia seeds, flax seeds, cucumber, and green tea.
Lifestyle
Stay active. This does not mean that you have to work out for one hour every day. Instead, try to get up and move your body throughout the day. You need to walk more and sit less. Perhaps, instead of watching TV on a couch, try to watch while standing. A 30-minute continuous activity is ideal.
Manage Adrenal PCOS
Adrenals are small triangular glands above our kidneys. They mainly produce cortisol, which is our primary stress hormone. These glands also secrete adrenaline (aka epinephrine), our fight or flight hormone (signal).
Stress can be likened to an alarm, it alerts us when there is a challenge or danger. When you lack sleep, lack sufficient food, grieving, are frustrated, threatened, are overworked, or have inflammation, your adrenals produce more cortisol and adrenaline to supply more sugar to your brain and create more anti-inflammatory substances.
Adrenaline is present when you feel excited or nervous. As per Wikipedia, adrenaline makes you more focused by temporarily dilating your pupils, expanding your airways, and improving memory recall.
Adrenals and PCOS
In connection to PCOS, the adrenals are responsible for the production of DHEA and Androgenic Steroids, which the ovaries convert to estrogen and androgen. Due to the consistent “sugar rush” produced by cortisol and adrenaline, chronic stress can also lead to insulin resistance and estrogen dominance. Both of these will trigger hormonal imbalance and will continue causing and worsening each other through a feedback loop.
When the adrenals are overactive (such as in Cushing’s syndrome) or under fatigue, the adrenals produce more androgenic steroids (testosterone) than needed, which results in male characteristics like hirsutism (hairy), baldness, or more masculinity. Testosterone also stimulates the oil glands and triggers acne.
Researchers have also found that cortisol levels are dysregulated among women with PCOS, which often translate to a higher waist-to-hip ratio and BMI.
If you have PCOS symptoms and chronic stress or Cushings, you might be suffering from Adrenal-type PCOS. Your doctor may ask you to undergo additional tests and imaging scans to confirm that your PCOS is caused by your adrenals or vice-versa. Until confirmation and proper prescription are available, you may want to make some diet and lifestyle changes to reduce stress and androgen.
Other Causes of High Cortisols
Growths or benign tumors (non-cancerous nodules/adenoma) in the adrenals or pituitary can cause overactive adrenals, which can increase stress and androgen levels. Note that adenomas often do not pose immediate health risks. However, they could affect hormone levels that can lead to PCOS.
Other possible causes of overactive adrenal glands are genetics and using prednisone (a steroid) for a prolonged period. Increased fat around the face or upper body fat accumulation, easy bruising, irregular cycles, and insomnia are some symptoms of Cushing’s apart from male-like features. High cholesterol is also common.
Medical Treatment
Armanini and colleagues (2007), studied the relationship between PCOS and androgen hormones. They suggested the use of spironolactone in patients with PCOS. Spironolactone acts as an anti-androgen -the only one approved in the US. It can limit the expression of male characteristics among women with PCOS. Often it takes at least 6 months to take effect.
According to MayoClinic, for women with PCOS and glucose intolerance Mifepristone (Korlym, Mifeprex) can help reduce cortisol uptake. For those with adenoma (tumor/nodule), surgical removal of the tumor or the gland is an option.
Diet
There are several herbs and food that have anti-androgenic effects, which you can incorporate into your diet. Licorice, green tea, white peony, and spearmint are the popular ones. Do not take in excess and if possible check with your doctor before consuming (especially if you are taking medications).
It is best to avoid processed and sugary foods, as well as excessive caffeine and alcohol because they can increase cortisol. In a 2021 study by M. Nemmeth and colleagues, guinea pigs given a diet high in saturated fats have higher cortisol.
Fatty fish, nuts, and mint can also help with stress. Among supplements, Vitamin D is highly recommended to decrease depression. Chamomile and valerian teas are traditionally been used to help calm the nerves. St John’s Worth was also suggested but it could result in photosensitivity and interact with hormonal pills.
Just be sure to take them at home or during night time because they can make some people drowsy. These can help manage your cortisol levels.
Eating on time (every 3-5 hours), or not letting yourself starve is another dietary change that you can consider. When blood sugar is low, the body produces cortisol. You can eat in small amounts if you are trying to lose weight. In Japan, they have a concept called Hara Hachi bu, which means eat only until you are 80% full.
Lifestyle
Apart from diet changes and habits, also consider listening to your body’s circadian rhythm. Do you know why it is difficult to sleep when you are stressed? Or how your body automatically wakes up in the morning? That’s cortisol at work.
If the adrenals are producing higher amounts of hormones, it may result in insomnia and moodiness. While it is best to sleep longer, try to get out of bed as soon as you wake up -that’s when you have a surge of cortisol. Then try to do some simple exercises like yoga or walking for at least 5 minutes to help level your cortisol.
Meditation and mindfulness practices are also effective in controlling stress. Relaxation techniques like breathing exercises, stretching, and yoga, can help shift your mind’s focus away from the stressor.
To start, try gratitude thinking whenever you feel stressed. Think of 3 things that you have or enjoy, that others may not have (ie. sleep, work, and food)
Another de-stressor is taking a warm bath or shower. Others swear by Epsom salt baths or foot soak. I usually do this when I sense my migraine is coming. It helps. The scents of lavender, peppermint, and rosemary are also popular for calming the senses.
Takeaway: Manage PCOS by limiting triggers
If your goal is to “reverse” or manage your PCOS, understanding its triggers or the factors that exacerbate its expression is key. There are different types of PCOS based on their causes, which require different management. Although, they overlap because of the feedback loop and domino effect caused by hormonal imbalance, focusing on managing the cause of the symptoms can help better than managing the effects of the symptoms.
Inflammatory PCOS is largely due to food intolerance. A family history of diabetes and a high-sugar diet is the main culprits for Insulin-Resistant PCOS. Synthetic PCOS is often a temporary side-effect of hormonal pills and other xenoestrogens from the environment. Finally, Adrenal PCOS may result from chronic stress or overactive adrenals.


